Why does Insulin Resistance matter if you’re not yet have symptoms and normal blood sugar?
One role of insulin is to help glucose in our blood to enter into skeletal muscle and fat tissue for storage. When blood sugar rises above the normal range (after a high carbohydrate meal for example), insulin is secreted to push the excess glucose into cells, bringing the blood sugar back down to a normal level. Insulin is the storage hormone. When it is around in the blood, it promotes storage of molecules in the form of fat in fat cells and some in muscle cells and liver. When insulin levels in the blood are high, your body cannot access the stored fat to use as energy. When insulin levels are low, your body can access stored fat and use it for energy.
When does insulin become a problem? Carbohydrates (and protein to a lesser extent) in the diet cause blood glucose levels to rise, which leads to a subsequent rise in insulin to help the body clear this excess glucose from the blood. When this goes on for a long time (like in someone consuming a typical diet that is high in carbohydrates), the cells start to become resistant to the effects of insulin. When this happens, your pancreas has to produce higher levels of insulin to get the same effect of lowering the blood glucose and getting the sugar into the cells. This is insulin resistance. This is occurring LONG before someone is ever diagnosed with prediabetes or diabetes. Why? Because for a long time, the body is still able to over-produce insulin to keep blood sugar levels within the normal range. This is a key point at which dietary and lifestyle intervention could easily reverse the path towards diabetes before it has occurred. At this point, insulin levels are chronically high in the blood. As mentioned above, insulin is the fat storage hormone. When it is around in high levels, the body is unable to access stored body fat to use for energy and continues to store fat. This results in a net fat gain and inability to burn fat usually despite calorie restriction. This is what drives metabolic syndrome.
What happens when high insulin levels continue?
Your pancreas can no longer keep up, your cells become increasingly resistant, and this is when your blood sugar levels start to rise. At this point, you are diagnosed as pre-diabetic or diabetic depending on how high your blood glucose levels are.
Who should be tested for Insulin Resistance?
The American Diabetes Association (ADA) recommends that testing to detect prediabetes be considered in adults who are overweight or obese and have one or more additional risk factors for diabetes. The section "Body Mass Index (BMI)" explains how to determine if a person is overweight or obese. However, not everyone who is overweight will get type 2 diabetes. People without these risk factors should begin testing at age 45.
Risk factors for prediabetes—in addition to being overweight or obese or being age 45 or older—include the following:
- Being physically inactive
- Having a parent or sibling with diabetes
- Having a family background that is African American, Alaska Native, American Indian, Asian American, Hispanic/Latino, or Pacific Islander American
- Giving birth to a baby weighing more than 9 pounds
- Being diagnosed with gestational diabetes—diabetes that develops only during pregnancy
- Having high blood pressure—140/90 mmHg or above—or being treated for high blood pressure
- HDL cholesterol level below 35 mg/dL or a triglyceride level above 250 mg/dL
- Having polycystic ovary syndrome (PCOS)
- Having prediabetes, impaired fasting glucose (IFG), or impaired glucose tolerance (IGT) on an earlier testing
- Having other conditions associated with insulin resistance, such as obesity or acanthosis nigricans
- Having Cardiovascular Disease
If test results are normal, testing should be repeated at least every 3 years. Testing is important for early diagnosis. Catching prediabetes early gives people time to change their lifestyle and prevent type 2 diabetes and CVD. Health care providers may recommend more frequent testing depending on initial results and risk status.
In addition to weight, the location of excess fat on the body can be important. A waist measurement of 40 inches or more for men and 35 inches or more for women is linked to insulin resistance and increases a person's risk for type 2 diabetes. This is true even if a person's BMI falls within the normal range.
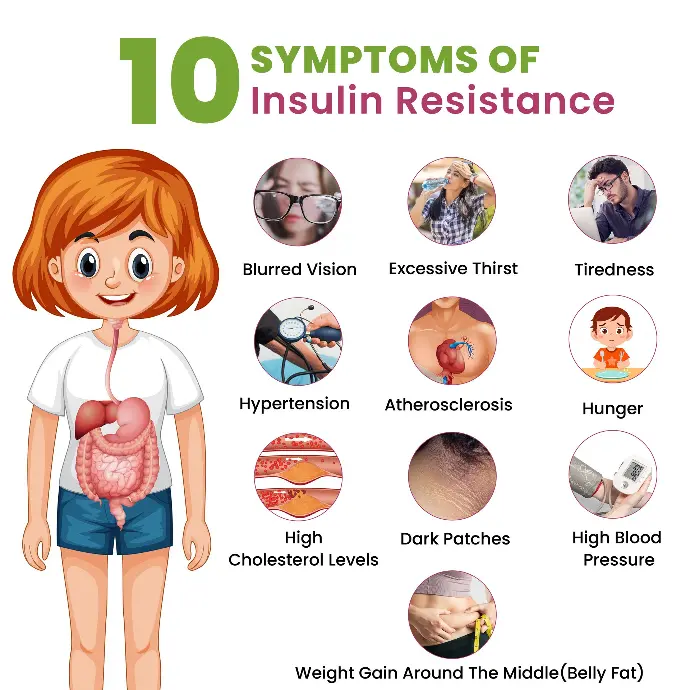
What are the symptoms of Insulin Resistance?
Insulin resistance and prediabetes usually have no symptoms. People may have one or both conditions for several years without knowing they have them. Even without symptoms, health care providers can identify people at high risk by their physical characteristics, also known as risk factors.
People with a severe form of insulin resistance may have dark patches of skin, usually on the back of the neck. Sometimes people have a dark ring around their neck. Dark patches may also appear on elbows, knees, knuckles, and armpits. This condition is called acanthosis nigricans.
What is Insulin?
Insulin is a hormone made in the pancreas, an organ located behind the stomach. The pancreas contains clusters of cells called islets. Beta cells within the islets make insulin and release it into the blood.
Insulin plays a major role in metabolism—the way the body uses digested food for energy. The digestive tract breaks down carbohydrates(sugars and starches)into glucose. Even Fructose is converted to Glucose. Glucose is a form of sugar that enters the bloodstream. With the help of insulin, cells throughout the body get glucose in and use it for energy.
Insulin's Role in Blood Glucose Control
When blood glucose levels rise after a meal, the pancreas releases insulin into the blood. Insulin and glucose then travel in the blood to cells throughout the body.
- Insulin helps muscle, fat, and liver cells absorb glucose from the bloodstream, lowering blood glucose levels.
- Insulin stimulates the liver and muscle tissue to store excess glucose. The stored form of glucose is called glycogen.
- Insulin also lowers blood glucose levels by reducing glucose production in the liver.
- Insulin is a critical regulator of virtually all aspects of adipocyte (Fat cells), and adipocytes are one of the most highly insulin-responsive cell types.
- Insulin promotes fat stores by stimulating glucose transport and triglyceride synthesis (lipogenesis), as well as inhibiting lipolysis
In a healthy person, these functions allow blood glucose and insulin levels to remain in the normal range with normal body weight.